Allergic rhinitis
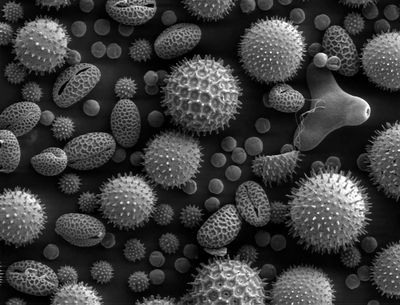 Pollen grains from a variety of common plants can cause hay fever. |
|
| ICD-10 | J30. |
|---|---|
| ICD-9 | 477 |
| OMIM | 607154 |
| DiseasesDB | 31140 |
| MedlinePlus | 000813 |
| eMedicine | ent/194 med/104, ped/2560 |
| MeSH | D012221 |
Allergic rhinitis, pollenosis or hay fever is an allergic inflammation of the nasal airways. It occurs when an allergen such as pollen or dust is inhaled by an individual with a sensitized immune system, and triggers antibody production. These antibodies mostly bind to mast cells, which contain histamine. When the mast cells are stimulated by pollen and dust, histamine (and other chemicals) are released. This causes itching, swelling, and mucus production. Symptoms vary in severity between individuals. Very sensitive individuals can experience hives or other rashes. Particulate matter in polluted air and chemicals such as chlorine and detergents, which can normally be tolerated, can greatly aggravate the condition.
Contents |
Classification
The two categories of allergic rhinitis include:
- Seasonal – occurs particularly during pollen seasons. Seasonal allergic rhinitis does not usually develop until after 6 years of age.
- Perennial – occurs throughout the year. This type of allergic rhinitis is commonly seen in younger children.[1]
Signs and symptoms
Characteristic physical findings in individuals who have allergic rhinitis include conjunctival swelling and erythema, eyelid swelling, lower eyelid venous stasis, lateral crease on the nose, swollen nasal turbinates, and middle ear effusion.[2]
Sufferers might also find that cross-reactivity occurs.[3] For example, someone allergic to birch pollen may also find that they have an allergic reaction to the skin of apples or potatoes.[4] A clear sign of this is the occurrence of an itchy throat after eating an apple or sneezing when peeling potatoes or apples. This occurs because of similarities in the proteins of the pollen and the food.[5] There are many cross-reacting substances.
Some disorders may be associated with allergies: Comorbidities include eczema, asthma, depression and migraine.[6]
Cause
Allergies are common. Heredity and environmental exposures may contribute to a predisposition to allergies. It is roughly estimated that one in three people have an active allergy at any given time and at least three in four people develop an allergic reaction at least once in their lives.
Allergic rhinitis triggered by the pollens of specific seasonal plants is commonly known as "hay fever", because it is most prevalent during haying season. However, it is possible to suffer from hay fever throughout the year. The pollen which causes hay fever varies between individuals and from region to region; generally speaking, the tiny, hardly visible pollens of wind-pollinated plants are the predominant cause. Pollens of insect-pollinated plants are too large to remain airborne and pose no risk. Examples of plants commonly responsible for hay fever include:
- Trees: such as pine , birch (Betula), alder (Alnus), cedar, hazel, hornbeam (Carpinus), horse chestnut (Aesculus), willow (Salix), poplar, plane (Platanus), linden/lime (Tilia) and olive (Olea). In northern latitudes birch is considered to be the most important allergenic tree pollen, with an estimated 15–20% of hay fever sufferers sensitive to birch pollen grains. Olive pollen is most predominant in Mediterranean regions.
- Grasses (Family Poaceae): especially ryegrass (Lolium sp.) and timothy (Phleum pratense). An estimated 90% of hay fever sufferers are allergic to grass pollen.
- Weeds: ragweed (Ambrosia), plantain (Plantago), nettle/parietaria (Urticaceae), mugwort (Artemisia), Fat hen (Chenopodium) and sorrel/dock (Rumex)
Allergy testing may reveal the specific allergens an individual is sensitive to. Skin testing is the most common method of allergy testing. This may include intradermal, scratch, patch, or other tests. Less commonly, the suspected allergen is dissolved and dropped onto the lower eyelid as a means of testing for allergies. (This test should only be done by a physician, never the patient, since it can be harmful if done improperly). In some individuals who cannot undergo skin testing (as determined by the doctor), the RAST blood test may be helpful in determining specific allergen sensitivity.
Management
The goal of rhinitis treatment is to reduce the symptoms caused by the inflammation of affected tissues. In cases of allergic rhinitis, the most effective way to decrease allergic symptoms is to completely avoid the allergen.[7][8] Vasomotor rhinitis can be brought under a measure of control through avoidance of irritants, though many irritants, such as weather changes, are uncontrollable.
Allergic rhinitis can typically be treated much like any other allergic condition. Eliminating exposure to allergens is the most effective preventive measure, but requires consistent effort. Many people with pollen allergies reduce their exposure by remaining indoors during hay fever season, particularly in the morning and evening, when outdoor pollen levels are at their highest. Closing all the windows and doors prevents wind-borne pollen from entering the home or office. When traveling in a vehicle, closing all the windows reduces exposure. Air conditioners are reasonably effective filters, and special pollen filters can be fitted to both home and vehicle air conditioning systems.[9]
Rinsing is very often recommended as part of the healing process after sinus or nasal surgery. For this rinse, boiled or distilled water is only necessary during recovery from surgery, as the entire contents of the bottle is used.[10]
Antihistamines
Several antagonistic drugs are used to block the action of allergic mediators, or to prevent activation of cells and degranulation processes. These include antihistamines, cortisone, dexamethasone, hydrocortisone, epinephrine (adrenaline), theophylline and cromolyn sodium. Anti-leukotrienes, such as montelukast, are FDA approved for treatment of allergic diseases.[11] One antihistamine, azelastine, is available as a nasal spray.
Many allergy medications can have undesirable side-effects, most notably drowsiness.
A case-control study found "symptomatic allergic rhinitis and rhinitis medication use are associated with a significantly increased risk of unexpectedly dropping a grade in summer examinations".[12]
Another study “suggests that drivers who need antihistamine drugs should avoid those that act centrally” because they “greatly impaired driving behaviour” [13]
Steroids
Systemic steroids such as prednisone are effective at reducing nasal inflammation, but their use is limited by their short duration of effect and the side effects of prolonged steroid therapy. Steroid nasal sprays are effective and safe, and may be effective without oral antihistamines. They take several days to act and so need be taken continually for several weeks as their therapeutic effect builds up with time.
Decongestants
Pseudoephedrine is also indicated for vasomotor rhinitis,
Topical decongestants: may also be helpful in reducing symptoms such as nasal congestion, but should not be used for long periods as stopping them after protracted use can lead to a rebound nasal congestion (Rhinitis medicamentosa).
Desensitization
More severe cases of allergic rhinitis require immunotherapy (allergy shots) or removal of tissue in the nose (e.g., nasal polyps) or sinuses.
Alternative treatments
Therapeutic efficacy of complementary-alternative treatments is not supported by currently available evidence.[14][15]
The World Health Organization places allergic rhinitis (including hayfever) on its list of diseases, symptoms or conditions for which acupuncture has been proven an effective treatment via controlled trials.[16]
Epidemiology
In Western countries between 10—25% of people annually are affected by allergic rhinitis.[17]
References
- ↑ "Rush University Medical Center". http://www.rush.edu/rumc/page-1098987384061.html. Retrieved 2008-03-05.
- ↑ Valet RS, Fahrenholz JM. Allergic rhinitis: update on diagnosis. Consultant. 2009;49:610-613
- ↑ Czaja-Bulsa G, Bachórska J (1998). "[Food allergy in children with pollinosis in the Western sea coast region]". Pol Merkur Lekarski 5 (30): 338–40. PMID 10101519.
- ↑ Yamamoto T, Asakura K, Shirasaki H, Himi T, Ogasawara H, Narita S, Kataura A (2005). "[Relationship between pollen allergy and oral allergy syndrome]". Nippon Jibiinkoka Gakkai Kaiho 108 (10): 971–9. PMID 16285612.
- ↑ Malandain H (2003). "[Allergies associated with both food and pollen]". Allerg Immunol (Paris) 35 (7): 253–6. PMID 14626714.
- ↑ "Allergists Explore Rising Prevalence and Unmet Needs Attributed to Allergic Rhinitis". ACAAI. November 12, 2006. http://www.acaai.org/public/linkpages/NR+Rising+Prevalence+and+Unmet+Needs+of+Allergic+Rhinitis.htm. Retrieved 2008-10-01.
- ↑ "The Facts about Hay Fever". Healthlink. University of Wisconsin. http://healthlink.mcw.edu/article/1031002426.html. Retrieved 2007-06-19.
- ↑ "NHS advice on hayfever". http://www.nhs.uk/Conditions/Hay-fever/Pages/Prevention.aspx?url=Pages/Lifestyle.aspx.
- ↑ Steven Jay Weiss. "Seasonal Allergic Rhinitis". http://www.suggestadoctor.com/health_article_28.htm. Retrieved 2009-01-28.
- ↑ Australian Society of Clinical Immunology and Allergy
- ↑ eMedicine Health Hay Fever Causes, Symptoms, and Treatment on eMedicineHealth.com
- ↑ Walker S, Khan-Wasti S, Fletcher M, Cullinan P, Harris J, Sheikh A (2007). "Seasonal allergic rhinitis is associated with a detrimental effect on examination performance in United Kingdom teenagers: case-control study". J. Allergy Clin. Immunol. 120 (2): 381–7. doi:10.1016/j.jaci.2007.03.034. PMID 17560637.
- ↑ T Betts, D Markman, S Debenham, D Mortiboy, and T McKevitt.. "Effects of two antihistamine drugs on actual driving performance.". http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1444070/. Retrieved 1984 January 28.
- ↑ Passalacqua G, Bousquet PJ, Carlsen KH, Kemp J, Lockey RF, Niggemann B, Pawankar R, Price D, Bousquet J (2006). "ARIA update: I--Systematic review of complementary and alternative medicine for rhinitis and asthma". J. Allergy Clin. Immunol. 117 (5): 1054–62. doi:10.1016/j.jaci.2005.12.1308. PMID 16675332.
- ↑ Terr A (2004). "Unproven and controversial forms of immunotherapy". Clin Allergy Immunol. 18 (1): 703–10. PMID 15042943.
- ↑ World Health Organisation (2002). Acupuncture: Review and Analysis of Reports on Controlled Clinical Trials. Geneva: WHO. 87. ISBN 9789241545433.
- ↑ Dykewicz MS, Hamilos DL (February 2010). "Rhinitis and sinusitis". J. Allergy Clin. Immunol. 125 (2 Suppl 2): S103–15. doi:10.1016/j.jaci.2009.12.989. PMID 20176255.